New Berkley School of Nursing Certificate Program Expands Access to Mental Health Care in Communities
(December 18, 2025) — To help address the nation’s escalating mental health needs, the Berkley School of Nursing has launched a Psychiatric Mental Health Nurse Practitioner (PMHNP) certificate program. The inaugural cohort of established post-master’s nurses are learning the necessary competencies to provide mental health services directly to their patients in primary and urgent care settings to fill the critical gap for care in communities.
The United States is facing an acute mental health crisis with approximately one in five adults living with a mental illness. Despite the demand for mental health providers, over 122 million people live in a designated Mental Health Care Health Professional Shortage Area, underscoring the urgency for more providers like those in the PMHNP program.
Program leaders and students share a common goal of being able to provide patients access to mental health services along with their other health care needs, and truly embody Georgetown’s mission of cura personalis or “care for the whole person.”
A Commitment to Community
Karan Kverno, PhD, PMHNP-BC, PMHCNS-BC, FAANP, FAAN
A defining feature of the certificate program is to build a sustainable local network of mental health care in Washington, D.C. As part of that goal, enrollment is limited to students who live in the area.
“We’re trying to make a difference with the program in our communities,” said Karan Kverno, PhD, PMHNP-BC, PMHCNS-BC, FAANP, FAAN, the program’s director. By focusing on local students, Kverno believes, the nursing school is fostering a system where providers can rely on students long after graduation. “It’s good for the community providers that our students partner with for clinical hours to know the students might stay in the area after completing the program,” she said.
Kverno, who balances her academic role with clinical practice at MedStar Union Memorial Hospital in Baltimore, emphasizes that the role of a PMHNP goes beyond the initial 30-minute mental health assessment. It also involves evaluating social circumstances, case management, and psychotherapy to help patients navigate stressful life circumstances.
Holistic Care: Facing Difficult Conversations
On a recent December afternoon at Georgetown’s Capitol Campus, Kverno and PMHNP students gathered around a conference room table to work through different interventions for hypothetical clients navigating domestic violence. The day prior, the students participated in a live simulation of a psychiatric evaluation with standardized patients as part of a two-day on-campus clinical intensive (OCI). The OCI is built into the PMHNP curriculum to help students develop the needed competencies in psychiatric assessment, diagnostic reasoning, and evidence-based interventions, as well as just learning how to interact with patients when asking sometimes difficult questions.
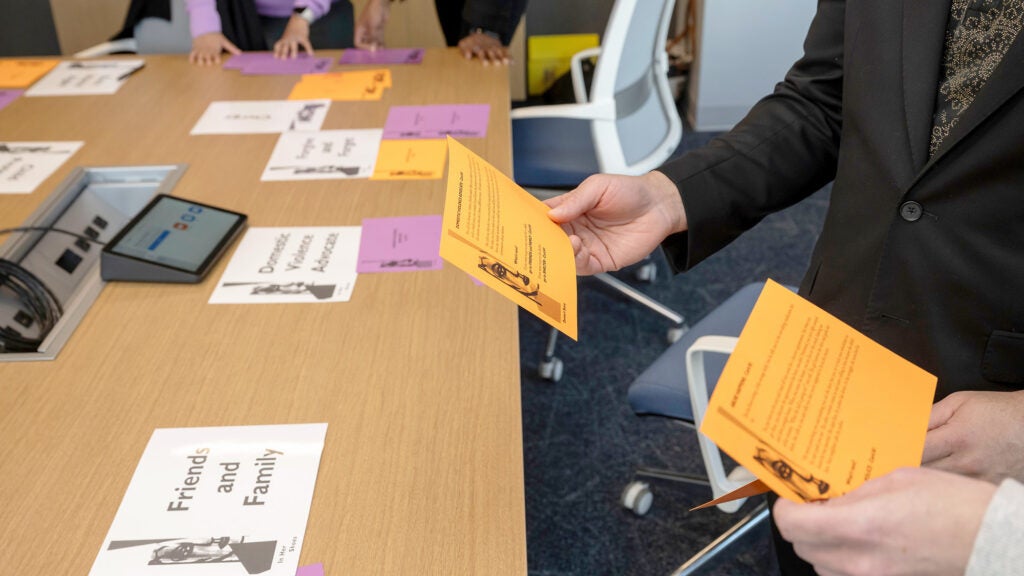
Students worked through different interventions for hypothetical clients navigating domestic violence at a recent OCI.
“The simulations were a great learning experience that really challenged us to reflect on how we handle ourselves when interacting with patients,” said Tyris Ford, CRNP. “The standardized patient feedback was insightful in sharing with us that they felt like we were just drilling them with questions instead of trying to have a conversation and connect more. Hearing that feedback is something I will definitely keep with me in the future.”
Ford specializes in sexual health and HIV care in his primary care practice. He decided to pursue psychiatric certification after identifying unmet needs within the LGBTQ+ and Black communities he serves. Ford found that proficiency in discussing sexual health histories often revealed underlying mental health struggles.

Tyris Ford, CRNP
“To me, you couldn’t go into HIV care without a focus on sexual health. To be effective with the community I serve, it’s important to talk sex, which can bring out other conversations” said Ford.
He relied on his skills as a nurse to sit with patients, listen to their stories and offer compassion when he could; but he wanted to be able to provide more for them. He was drawn to Georgetown’s PMHNP program because of its emphasis on psychotherapy and caring for the “whole person,” rather than a medication management approach to care.
“I didn’t want to study just ‘traditional psychiatry,’ where I’m just a prescriber sending them on their way to monitor a response to medicine,” Ford explained. “Many of my patients don’t want to go to a psychiatrist. With this program, I’m building the skills necessary to meet my patients where they are at, and help them build healthier habits.”
The Personal Journey to Psychiatry
Dristi Basnet, a nurse practitioner, dedicated herself to pediatric primary care after witnessing the vulnerability of children in refugee camps, an experience she lived through personally when her family fled Bhutan in 1999 for a refugee camp in Nepal.

Dristi Basnet, PNP
“In the refugee camps, I saw profound medical needs. Kids were not getting fed, and it was a lot to see at a young age,” Basnet said.
However, while working in pediatric primary care in the United States, primarily with immigrant families, she encountered a different kind of crisis when her patients were placed on endless waitlists for mental health services. “For many immigrant families, mental health is rarely discussed, which contributes to the compounding need for integrated care including mental health in their primary health care setting, where families are already coming for care and feel safe in that setting.”
“I think there is value in being able to expand our knowledge in primary care,” Basnet said. “If a child comes in for a physical appointment and has a high depression score, I want to manage that at the clinic rather than handing it off,” she said.
For Basnet, the ability to treat rather than just refer is transformative. “Just the fact that I can manage it better, not just in my clinical work experience, but for the community, that’s incredibly valuable.”
Bridging the Gap in Urgent Care
For Hilary Summers-Royce (G’13), an FNP with 12 years of experience, the path to psychiatry was a “second career” sparked by personal experience. While her husband was deployed to Afghanistan, Summers-Royce transitioned from the business world into nursing, eventually working in an urgent care setting. It was there that she experienced a “lightbulb moment” regarding the limitations of her scope of practice.

Hilary Summers-Royce, FNP (G’13)
“Patients would come in for a sinus infection, but then score positively on depression screenings,” said Summers-Royce. “I felt like I lacked the knowledge to follow through. My goal now with the PMHNP program is to be able to dig in and provide the additional help and knowledge they need.”
She credits Georgetown for helping her connect the dots between physical ailments and mental well-being. “Georgetown is about treating the whole patient. Cura personalis is helpful in thinking about the right questions to ask, not only about physical ailments but also about their mental health.”
A Supportive, Intimate Cohort
The program’s small size fosters a personalized learning environment where students rely on one another, especially when confronting difficult topics. “We started a group text among the four of us, supporting each other through the whole program,” Basnet said.
As the cohort moves forward, they carry a shared outlook about the program summarized by Ford: “There are very few programs that genuinely embrace the mind, body, emotion and mental health. Georgetown really stands out in its approach to care that’s uniquely holistic.”
Heather Wilpone-Welborn
GUMC Communications

